Annual Regulatory Requirements, Current Practice - 2.5 Contact Hours
This course is approved through the California Board of Registered Nursing Provider #CEP 13509.
Course Outline
- Outcomes
- Objectives
- Introduction
- Statutory versus Mandatory
- Knowing Client's Rights
- Access to Emergency Services Training
- Information Disclosure to Clients
- Workplace Safety
- Recognizing and Reporting Abuse
- Use of Restraints
- Violence Preparation
- Radiation Safety
- Environment Safety
- Infection Prevention
- Hand Washing Guidelines
- Standard Precautions
- Personal Protective Equipment (PPE)
- Needlestick Prevention
- Transmission-Based Precautions (Isolation)
- Contact Precautions
- Airborne Precautions
- Droplet Precautions
- Neutropenic Precautions
- Central Line and Surgical Infections
- Infectious Waste Management
- Recommended Healthcare Worker Immunization
- Exposure to Bloodborne Pathogens
- Pain Management
- Hazardous Flammable Combustible - Liquids, Vapors, and Gases
- Antineoplastic Drugs, Hazardous Drugs, Toxic Substances
- Electrical Safety
- Waived Testing
- Conclusion
- References
Outcomes
≥ 92% of participants will know the current annual training topics required for the Healthcare Insurance Portability and Accountability Act (HIPAA), the Joint Commission on Accreditation of Healthcare Organizations (TJC), and the Occupational Safety and Health Administration (OSHA).
Objectives
After completing this course, the learner will be able to:
Relate the importance of required training.
Describe training related to the Joint Commission on Accreditation of Healthcare Organizations (TJC).
Infer training points related to Healthcare Insurance Portability and Accountability Act (HIPAA) regulations.
Specify training related to a safe workplace.
Construct training with an infection prevention focus.
Introduction
Quality healthcare includes a responsibility to many masters, of which the client is number one. Have you ever wondered, though, who looks out for the client? Who ensures everything is up to date and running smoothly, and how do they accomplish the massive task of ensuring that health professionals provide the best possible care?
The answer is we all work together towards quality care. All healthcare professionals work toward the goal of providing the best care, and to help us on this mission, we look for
Please be mindful that regulatory agencies are not an enemy, nor are they choosing to unduly burden you with repetitive classwork through which you can nap. The viewpoint across the horizon of healthcare, comparing desired outcomes to reality on regional, national, and even international levels, shows vulnerabilities and the need for improvements that we may not be aware of. That broader view can also identify real-to-us skills that need honing or information deficits we are unaware of.
Statutory versus Mandatory
There is overlap, creating great confusion, so we will begin with some simple definitions.
| Statutory Training | |
| Mandatory Training | It tends to be set by an organization for its people, specifically for a particular workplace work environment. |
| Required Training | Training for health care providers may be statutory, mandatory from the employer, or both. The local training you must take often addresses mostly current, local issues while containing a portion required by an outside agency. |
(McPheat, 2023; Mundey, 2023)
Statutory training, therefore, consists of the requirements of an organization to meet legal or contractual requirements. The Joint Commission, for example, is a private corporation requiring certain elements to be met to deem that a hospital or care system is TJC Certified. At the same time, mandatory training refers to those classes and opportunities for practice determined by an employer to meet a policy or standard of practice.
It is important to note that while mandatory and statutory training might overlap and, in some situations, even be merged, they are not interchangeable.
Clear as mud? Here is an example.
| Terry shook her head in disbelief. She had to complete two fire safety classes! Wasn’t management aware of how short-staffed they were? One was online, which was not so bad, but the other was in-person training! Of all the time wasted! Well, she could knock them both out tomorrow afternoon. She would do the online training first, then mock the in-person instructor by knowing all the answers! |
| That was not what she expected, Terry thought ruefully after the training. There was some overlap, yet the two classes were widely different. The mandatory online, virtual training was mainly about organization policies, procedures, and practices. The live training focused on statutory items such as Occupational Safety and Health Administration (OSHA) guidelines and focused on practical skills. She could even pull a real (for practice) fire alarm and spray down a mock fire with a fire extinguisher! Wow, how cool! She had never thought a fire extinguisher would buck in her hands when she pulled the trigger like that! It was fun, and she learned fundamental skills from it! |
(McPheat, 2023; Mundey, 2023)
Knowing Client's Rights
What health workers do is all about the patient and the client. Unsurprisingly, several regulatory agencies bring clients’ rights to the forefront of annual required training for healthcare professionals. Definitions and concepts of a client's rights and the idea that a client might possess any rights have dramatically changed over the last few decades. Be warned that client rights, privileges, and clients' duties, and obligations remain in a state of societal flux. The anticipation is that changing perspectives will continue for some time, making this a smart topic under regulatory scrutiny and requiring regular training updates.
In its broadest sense, client rights define the basic rules of conduct between healthcare personnel and their clients. This includes institutions and health systems and those employed in any capacity to serve them. Details concerning client rights can be found anchored in federal regulatory documents such as the Emergency Medical Treatment and Active Labor Act (EMTALA), as well as in every health profession’s defining articles, such as the American Medical Association (AMA) Code of Medical Ethics (Smith, 2023). Concepts and details concerning client rights abound in state and federal legal statutes and, if broken, may result in professional suspension, fines, or even prison.
When discussing client rights training, it seems easier to ask, who does not require healthcare professionals to update their knowledge on this topic? Two of the major regulatory and accreditation organizations that require frequent and annual patient rights training are.
- CMS (Center for Medicare/Medicaid Services).
- TJC (The Joint Commission).
Information Disclosure - Y
ou have the right to receive accurate information that you can understand about your health, treatments, health plan, health care providers, and health care facilities. If you speak another language, have a physical or mental disability, or do not understand something, you will be helped to make informed healthcare decisions.Choice of Providers and Plans - You can choose your health care provider within your health plan.
Access to Emergency Services - If you have severe pain, an injury, or sudden illness and you are concerned that you could be seriously ill, hurt, or could die, you have the right to get emergency services whenever and wherever needed, to be seen by a doctor, and get services, even if you do not ask your health plan first. You will not be charged a penalty.
Participation in Treatment Decisions - You have the right to know all your treatment options, even if your health plan does not cover them, and make decisions about your care. Parents, guardians, family members, or others that you choose can represent you if you cannot make your own decisions.
Respect and Nondiscrimination - You have the right to considerate, respectful care and not be discriminated against by your doctors, other health care providers, or health plan representatives.
Confidentiality of Health Information - You have the right to talk in private with health care providers and to have your health care information protected. You also have the right to review and copy your medical records and ask your doctor to correct your record if it is inaccurate, incomplete, or has information that does not relate to your health care.
Complaints and Appeals - You have the right to a fair, fast, and objective review of any complaint you have against your health plan, doctors, hospitals, or other health care personnel. This includes complaints about waiting times, hours available, healthcare facilities, and the conduct of healthcare personnel.
Additional consumer benefits are included.
- Insurance must accept you even if you have a pre-existing condition.
- Health plans must provide free basic preventive care.
- Adult dependents have the right to stay on their parent’s health plans until 26.
- Health plans may not limit yearly or lifetime coverage of essential benefits.
- You have the right to receive easy-to-understand information about your health benefits.
- Protections exist from unreasonable insurance rate increases.
- You have the right to appeal to a health insurance company decision.
Consumer Responsibilities.
- Do your best to get well and stay healthy with healthy habits, such as exercising, not smoking, and eating a healthy diet.
- It is imperative to communicate what you want and need clearly.
- Be involved with your health care providers when making health care decisions.
- Work with healthcare providers to develop and conduct your agreed-upon treatment plans.
- Use the health plan's internal complaint and appeal process to address possible concerns.
- Avoid knowingly spreading disease.
- Recognition of risks and limits of the science of medical care and that healthcare providers are human and can make mistakes.
- Be aware of a healthcare provider's need to provide care fairly to other patients and the community.
- Learn about your health plan coverage and options (when available), including all covered benefits, the limits, what is not covered, the rules regarding the use of information, and how to appeal coverage decisions.
- Show respect for other patients and healthcare workers.
- Make a good-faith effort to pay your health care bills.
- Follow procedures of the health plans and health care providers.
- Report wrongdoing and fraud to the right resources or legal authorities.
Confidentiality of Health Information and HIPAA
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC IM.01.01.03 EP.3 | |
| TJC IM.03.01.01 EP.1 | Education and ongoing training on providing access to information resources 24/7. |
(JCR staff, 2024a)
Information about both clients and staff must be kept secure and confidential. Specific staff should be designated to ensure this, and any staff member working with client information must know how to maintain and secure protected information. This is not the job of medical records staff; it is everyone’s duty.
| Agency Regulation | Annual Required Training |
|---|---|
| OSHA 29.CFR.1910.1020(g) | Annual Exposure and Medical Records Training |
(Chambers, 2023; OSHA, 2023a)
Let’s face it; you cannot discuss patient rights without serving up a side of HIPAA. The Joint Commission, CMS, and many state and federal agencies require all healthcare staff, from pathologists to plumbers, to be regularly versed on relevant aspects of the Health Insurance Portability and Accountability Act (HIPAA).
The rule sets standards for patient privacy and confidentiality. It also sets severe civil and criminal penalties for people who violate a patient’s privacy. To comply with HIPAA, protected patient information must only be shared with people directly involved in that patient’s care. This is especially important when talking in public areas (elevators, restrooms, hallways, cafeterias, etc.). Charts or documents should not be left out where unauthorized persons might see them; computer screens should not be angled in such a way as to allow unwanted viewing. It is vitally important to observe surroundings when discussing patient care.
The privacy rule standards address the use and disclosure of individuals’ health information called “protected health information.” All facilities must limit access to protected health information only to those who need to know. A nurse seeking information about a patient not under their care violates the HIPAA rules. Protected health information can only be used for health purposes. Employers cannot use health history information to screen candidates for hire or promotion. Financial institutions may not use it to determine lending practices. Only the individual can explicitly authorize employers, banks, and individuals to have access to their medical information.
| Agency Regulation | Annual Required Training | |
|---|---|---|
| CMS 45 C.F.R. § 164.308(a)(3) & (4) | Ensure that all workforce members have appropriate access to electronic protected health information (ePHI), and prevent those members who do not have access to ePHI. Implement policies and procedures for authorizing access to ePHI. |
|
| CMS 45 C.F.R. § 164.308(a)(5)(i) | Train ALL workforce members regarding HIPAA security policies and procedures. | |
The HIPAA Privacy Rule protects individually identifiable personal health information, called PHI, held or transmitted by a covered entity or its business associate in any form, whether electronic, paper, or verbal. PHI includes information that relates to the following:
|
||
(CaseText Staff, 2023)
HIPAA also established the “minimum necessary rule,” which stipulates that only the minimum necessary information may be shared, even with the patient's authorization. A classic example would involve treatment for a case of child or domestic abuse; the professional would, rather than providing an entire medical record, share the pertinent data furnished in the form of an abstract outlining the information that is necessary to provide treatment and protect the victim. The abstracted information could be provided to legal and law enforcement entities.
- Emergency 911 situations
- When infectious diseases are involved
- When law enforcement agencies participate
- If national defense or security is a factor
The public health department is deemed a legitimate recipient of certain personal health information, and professionals may occasionally report certain findings to the proper public health agency. Included are the cause of death even when the patient dies at home, reportable communicable diseases, child abuse, reporting an adverse drug reaction to the Federal Drug Administration, the occurrence of cancer in a state with a cancer registry, meningitis, and immunizations for children.
| Agency Regulation | Annual Recommended/Required Training |
|---|---|
|
OCR (Office of Civil Rights) HIPPA 45 CFR § 164.308 |
Train all workforce members who work with personal health information (PHI) or electronic personal health information (ePHI).
|
| CMS 45 C.F.R. § 164.308(a)(5)(i) | Train ALL workforce members regarding HIPAA security policies and procedures. |
The HIPAA Privacy Rule protects individually identifiable personal health information, called PHI, held or transmitted by a covered entity or its business associate in any form, whether electronic, paper, or verbal. PHI includes information that relates to the following:
|
|
| *NOTE: Like many government rules, specific intervals required for HIPAA training are nebulous and will be held against both person and organization in case of an information breach. The best advice is to train all employees on both HIPAA Privacy and the HIPAA Security Rule annually. In The HIPAA Journal, December 20, 2023, HIPAA insider Steve Alder recommends twice yearly training for all healthcare support staff and strong record keeping of this training. | |
(Alder, 2023; HHS, 2023a)
HIPAA privacy regulations also mandate specific patient rights that include the following:
- Right to privacy notice requires disclosure and reasonable effort to ensure that the patient understands the agency’s policy concerning privacy of information.
- Right to request restrictions - patients may specify health information that cannot be released and may restrict to whom information can be released.
- Right to access personal health information - patients must be allowed to inspect and copy information in the agency’s record.
- Right to know what disclosures have been made - the agency must track all information released and be able to provide documentation to the patient.
- Right to amend personal health information - while patients may request amendments and the agency must allow amendments, the agency may deny some requests.
Electronically generated, stored, or transferred information also falls under HIPAA privacy rules. Both individuals and facilities are responsible for defending electronic protected health information (ePHI).
| Agency Regulation | Annual Required Training |
|---|---|
| CMS 45 C.F.R. § 164.530(b) | A covered entity must train ALL members of its workforce on the policies and procedures concerning protected health information. |
| The Security Rule specifies safeguards that covered entities and their business associates must implement to protect the confidentiality, integrity, and availability of ePHI. Covered entities and business associates must develop and implement policies and procedures to safeguard the security of PHI and electronic (aka) ePHI that they create, receive, maintain, or transmit. Each entity must analyze the risks to the ePHI in its environment and develop solutions appropriate for its situation. | |
(Alder, 2023)
Protected information that is shared, either by accident or with purpose, must immediately be reported using the facility's established procedures. Depending on the extent of the information breach, the federal agency overseeing HIPAA accountability and local media may need to be notified.
| Agency Regulation | Annual Required Training |
|---|---|
| CMS 45 CFR 164.530(b)(2)(ii) | ALL employees will receive regular training in HIPAA policies and procedures, PHI, ePHI, and Privacy breaches. |
| While the Privacy Breach Notification Rule does not explicitly require annual training, many experts in the field of compliance heartily recommend annual ALL staff training due to the risks and penalties associated with security and privacy violations. A privacy breach requires covered entities to notify affected individuals, the Department of Health and Human Services (HHS), and, in some cases, the media of a breach of unsecured PHI. Most notifications must be provided without unreasonable delay and no later than 60 days following the discovery of a breach. Notifications of more minor breaches affecting fewer than 500 individuals may be submitted annually to HHS in a log or other documentation. The Rule also requires business associates of covered entities to notify the covered entity of breaches at or by the business associate. The HHS Office for Civil Rights enforces the HIPAA Privacy, Security, and Breach Notification Rules. For more information on the enforcement process, visit the HHS website. Violations may result in the imposition of civil monetary penalties. In some cases, criminal penalties may apply, enforced by the Department of Justice. |
|
(Ting, 2023)
Access to Emergency Services Training
Several regulatory agencies require annual training regarding the ability of clients to access emergency care; this is especially important to CMS. The 1986 Emergency Medical Treatment and Labor Act (EMTALA) reflects the right to care, which ensures that the public has access to emergency services regardless of lack of insurance or ability to pay.
| Section 1867 of the Social Security Act imposes specific obligations on Medicare-participating hospitals that offer emergency services to provide a medical screening examination (MSE) when a request is made for examination or treatment for an emergency medical condition (EMC), including active labor, regardless of an individual's ability to pay. Hospitals are then required to provide stabilizing treatment for patients with EMCs. If a hospital cannot stabilize a client within its capability, or if the patient requests, an appropriate transfer should be implemented. |
Suppose the client has severe pain, an injury, or a sudden illness that convinces them that their health is in serious jeopardy. In that case, they have the right to receive screening and stabilization emergency services whenever and wherever needed without prior authorization or financial penalty. The client has the right to request a transfer to another institution, providing it is medically permissible, and the other facility will accept the transfer.
Under EMTALA, a hospital must screen all incoming clients. The screening must be complete enough to determine whether that person has an emergency medical condition. The medical screening exam must be performed by a physician or qualified individual designated by the facility to provide the medical screening exam.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC HR.01.05.03 | Education and training on identifying and responding to patient condition changes. NOTE: Training frequency is not specified in this requirement; however, compliance professionals tend to advise annual training of designated personnel with good record keeping. |
(JCR Staff, 2024b)
Please note all training involving EMTALA must clearly state that a triage exam does not constitute a medical screening exam.
If the client does not have an emergency condition, the hospital has no further obligation under EMTALA. The hospital must provide stabilizing treatment if the client has an emergency (Warby et al., 2023). This treatment must be provided without considering the client’s ability to pay. Before the client is stabilized, the hospital may transfer them out only if another facility is better equipped to treat them and their condition. A hospital may not transfer an unstable client for purely economic reasons.
Information Disclosure to Clients
Clients in healthcare facilities have the right to accurate and easily understandable information about their health plan, healthcare professionals, and the facility itself. Is English not their primary language, or do they have physical or mental disabilities? Appropriate information must be provided to allow them to make informed healthcare decisions.
Clients have the right to know about the facility itself. This information can cover a broad topic range, such as:
- How to file a complaint.
- The facility’s position on withholding and withdrawing life-sustaining care and treatment.
- Experience with specific procedures and services.
- Accreditation status, quality, and consumer satisfaction ratings – This information is available online.
- Their healthcare team – who is responsible for their care – names and professional status, team members' education and board certification status, years of practice, experience, quality, and consumer satisfaction ratings.
- Their rights and responsibilities as clients. Remember, they must understand the information they are given about their rights.
Auditing agencies understand that each facility will have its methods for ensuring clients know and understand their rights; regulatory agencies require proof that facilities provide this information. Inspection of expectations comes by direct observation and examination of facility policies or records.
Most facilities display information on client rights at intake points to the facility. Many also provide clients with a written form of rights at intake during the admission process in client handbooks. Rights and responsibilities may also be posted in waiting areas; be aware that a written list of rights is insufficient. The facility must ensure all clients understand their rights well enough to exercise them. This is true of all information. All information must be presented so that the person can understand it. This means that clients may need special help if they do not speak English, cannot see or hear well, or have other mental or physical barriers to understanding. Examples of special help include:
- Translation services.
- Sign-language interpreters.
- Social workers or case managers.
- Large print or Braille materials.
- Magnifying glass or large print documents.
Participation in Treatment Decisions Training
Clients have the right to participate in decisions about their care and to set the course of their treatment. This means that they must be given accurate information. They have the right to know their diagnosis, prognosis, and treatment options. Healthcare providers must discuss all treatment options with their clients, which includes the option of no treatment. Further, they must know each treatment option's risks, benefits, and potential medical consequences.
Informed Consent
Discussing clinical information with a client is part of informed consent. Informed consent is an ongoing communication process between a healthcare provider and the client. It allows the person to make intelligent decisions about a proposed course of treatment. Remember, information is useful to clients only if they can understand it. When discussing diagnosis and treatment options with the client, avoid the use of medical jargon and terminology, seek the services of a translator or interpreter if necessary, and assist the patient in obtaining a second opinion if requested.
After receiving all pertinent information, a client may consent to or refuse treatment. Signing as a witness on the informed consent document is witnessing that the client signed the document. It does not mean that the witness participated in providing informed consent.
Except in an emergency, a client must give informed consent before starting any procedure or treatment. Informed consent or the reason for a client’s inability to provide informed consent must be documented in the medical record. The informed consent document must:
- Be worded in simple terms without abbreviations.
- Indicate the specific procedure to be performed.
- Include a list of complications.
- Be written as stated in physician orders.
- Be signed by the client before receiving pre-op meds that induce sedation or amnesia or reduce anxiety.
- Contain the client’s dated signature if the client is of age and competent.
- Contain the signature of the physician performing the procedure.
- Ensure that the consent has a date and time.
- Include a witness’ signature affirming the client's signature.
Please note that two witnesses are required for the following:
- A person signing for an incompetent patient.
- Telephone consent.
- Signature of “X” if the client cannot write.
- When there is a clause for photographs and blood transfusion if applicable.
If the client cannot consent, laws vary from state to state, and policy varies from facility to facility. The following are accepted practices. The legal guardian must sign the consent if the client is a minor. An emancipated minor can sign consent. An emancipated minor is usually recognized as one who is not subject to parental control, as in the following situations:
- Married minor.
- In military service.
- College students are under legal age but are living away from home.
- Minor who has a child.
- Court-ordered emancipated minor.
If the client is incompetent or incapacitated, permission can be sought from a patient representative, usually a family member or Power of Attorney. An incompetent client is any client who is mentally or physically incapacitated, as determined by physicians, such that the client cannot communicate treatment preferences. The client does not have to be found incompetent by a court of law to consent to a procedure. Facility policy usually dictates the process and how many physicians must be involved in the decision.
In an emergency where the physician feels that delaying a procedure would be an immediate threat to the client’s life or limb, and the client cannot consent, the physician may proceed with the procedure without consent. This process requires extensive documentation and often a consultation with other physicians. Check your facilities policy.
Clients have the right to refuse treatment. Even after giving informed consent, the client may change their mind anytime. If the client decides to withdraw consent, the treatment must be stopped. Clients who refuse treatment have the right to know what will happen. They should receive information on medical and other consequences of refusing treatment. Parents, guardians, family members, or others designated as the client's representative must be provided with the same information if he cannot make their own decisions.
Advanced Directives
The Patient Self Determination Act became effective in December 1991 (GovTrack.us, 2024). This federal law requires that all hospitals receiving Medicare or Medicaid funding provide information to all adult clients upon admission about advanced directives and to ask whether they have an advanced directive. By federal and state regulations, clients should receive information regarding advanced directives if they do not present it upon admission. Advanced directives can be used from admission to admission; however, they should be reviewed with the client at each admission to verify accuracy.
The surrogate or proxy should provide information if the client is incompetent at admission. If the client is temporarily incapacitated, the information should be provided when decisional capacity returns. A client’s right to make decisions about their care is true even after they can no longer communicate those decisions directly. Advance directives can protect people who may be unable to communicate due to a condition such as irreversible brain damage or brain disease that affects the ability to think as well as communicate.
Advanced directives can limit life-prolonging measures when there is little or no chance of recovery. For example, advanced directives may enable clients to make their feelings known about cardiopulmonary resuscitation (CPR), intravenous (IV) therapy, feeding tubes, ventilators, respirators, and dialysis. Advanced directives can address pain relief, either requesting or refusing it.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC PC.02.01.11 EP.4 | Education and training on resuscitation equipment and techniques and proper need and use. |
| CMS 482.13(B) | All staff are trained on orientation at least every two years whenever policy/procedure changes on advance directives. |
| CMS 489.102(5) | Providing education to staff concerning its policies and procedures on advance directives – frequency not specified yet annually has been recommended. |
(CFR, 2024; CMS, 2023a; JCR Staff, 2024c)
- Living Will: a client documents their wishes for future treatment in the event of a terminal illness. A living will takes effect when a client develops a terminal condition that makes it impossible to communicate healthcare decisions directly. They are called living wills because they take effect while a client is alive.
- Durable Power of Attorney for Healthcare: the client appoints a representative to make healthcare decisions in this document. The power of attorney goes into effect when the client loses the ability to communicate their own decisions. The client names a person called a surrogate or proxy to make decisions.
An additional tool for participating in future healthcare decisions is the do-not-resuscitate (DNR) order. A DNR order states that a client does not want CPR if they go into cardiac or respiratory arrest. A client may request a DNR order; however, only a physician can approve and give the order.
To be clear, an advanced directive takes effect only after the client can no longer communicate directly. Until then, the client’s direct communication was the only thing that mattered. A competent client may change their advanced directive at any time. If a client wishes to change a directive, the healthcare professional must make it possible. Care must never be based on whether the client has an advanced directive and the decisions in the directive. All clients must be treated fairly and equally, regardless of advanced directives.
Power of attorney, drafted by a licensed attorney, is when one person authorizes another person to act on one’s behalf. Some important points regarding a power of attorney include signatures of the principal party, two adult witnesses, and the notary public. It may be used immediately. A power of attorney does not need to be filed in court except for real estate transactions. A power of attorney is in effect until revoked by the principal, participant’s death, or revoked by the court. A power of attorney may have more than one agent. If so, all agents must concur when making decisions. There are several types of power of attorney.
- General: an agent acts on behalf of the person in a variety of situations
- Limited: limited to a specific transaction
- Healthcare: to make decisions when incapacitated
- Springing: in effect at some future time – illness, disability of the principal
- Durable: all the above can be made “durable” by adding text – that enables the agent to act when the principal is incompetent and physically unable to make decisions
A healthcare surrogate is any competent adult expressly designated in writing by a client to make healthcare decisions on their behalf when incapacitated. This surrogate has no authority to act until the primary care physician determines that the principal cannot make informed healthcare decisions. A proxy is a competent adult who has not been expressly designated to make healthcare decisions for a particular incapacitated individual but who, nevertheless, is authorized to make healthcare decisions. A healthcare proxy is appointed by the hospital when there is no power of attorney or surrogate and healthcare decisions need to be made. Potential representatives for an incapacitated patient may include:
- Guardian
- Adult child
- Domestic partner
- Sibling
- Close friend
When clients often lose the ability to communicate directly, they do not have an advanced directive. The hierarchy of healthcare decision-makers for a client without an advance directive depends upon state law.
Research Participation
Clients have the right to be part of research studies or educational activities. If a client refuses experimental treatment, this should not affect their regular care. If the client wants to be part of a research study, they must sign a written consent explaining that the proposed treatment is experimental. The consent form for experimental treatment must include the nature of the experimental treatment, procedures involved, risks and benefits, other available options, and confirmation of any interruption in client care.
Organ Donation
| Agency Regulation | Annual Required Training |
|---|---|
| CMS 42 CFR § 482.45 | Organ, tissue, and eye procurement training for physicians and designated personnel. |
(CMS, 2023a)
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC TS.01.01.01 | Education and training on organ donation issues for physicians and any involved personnel. Issues include organ procurement organizations (OPO), the need for discretion, and sensitivity to beliefs and circumstances regarding the family of potential organ donors. |
(JCR Staff, 2024d)
Complaints, Grievances, and Appeals
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC PC.01.02.09 EP.3 | The organization educates staff about how to recognize signs of abuse, neglect, and exploitation and about their roles in follow-up, including reporting. |
| CMS 482.13(a)(2)(i) | All patient care staff are trained in orientation and whenever policy/procedures change on the grievance process. |
(CMS, 2023a; JCR Staff, 2024c)
Every client has the right to a fair, fast, and objective review of any complaint that they have concerning the health plan, doctors, hospital, or other healthcare personnel. This includes complaints about waiting times, operating hours, healthcare personnel's conduct, and healthcare facilities' adequacy. Many facilities have a client care representative to deal with complaints or grievances. Many client complaints can be addressed quickly. For example, if a client complains about getting the wrong items on her lunch tray, make sure she gets the right items next time. The sooner the issue is resolved at the lowest level possible, the better client compliance and satisfaction with the healthcare provider. The client may need access to the ethics committee for issues regarding their care. They should expect that issues related to end-of-life care be treated with respect and sensitivity. The client should be able to examine and receive an explanation of their bill regardless of the payment source.
More than 50% of the clients who sue do so because of miscommunications, anger, and lack of information between physicians, hospital staff, and clients/families. Grievance management is everyone’s responsibility. Handling grievances effectively from the start benefits everyone involved, helps keep minor grievances from becoming big ones, and reduces the risk of liability. When complaints cannot be resolved quickly and easily, clients have the right to file a grievance. A grievance is a formal, written, or verbal complaint. If a client wants to file a grievance, the healthcare professional must:
- Explain the grievance process at the facility. This includes the name of the staff person the client should contact for assistance resolving their grievance.
- Explain that grievances may be filed with state agencies. This is true whether the client has already used the facility’s internal grievance process.
- Give the client the phone number and address to file a grievance with the state.
Healthcare facilities must review, investigate, and resolve all grievances within a reasonable period. If the grievance has to do with the client’s safety, it should be reviewed immediately. Examples include grievances about abuse or neglect. The facility must give the client a written report to complete the grievance process. This report should explain how the facility investigated the grievance and the facility’s decision about the grievance.
Bills and Bill Examination
On a related note to HIPAA and grievances, clients can question their bills. They have the right to request and receive a detailed explanation of every item on a bill. Training on this subject is expected separately or as a component of client rights training.
Workplace Safety
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC APR.09.02.01 EP.1,2 | Address staff concerns about safety and quality of care, reporting ongoing training. |
(JCR Staff, 2024e)
Did you know that The Joint Commission is one of five hospital and health services accrediting agencies accepted by CMS for the United States? These accrediting agencies include The Joint Commission (TJC), the Healthcare Facilities Accreditation Program (HFAP), the Accreditation Association for Hospitals Health Systems Inc. (AAHHS), the Center for Improvement in Healthcare Quality (CIHQ), and Det Norske Veritas Healthcare Inc. (DNV).
TJC is the primary agency, providing oversight for more than 5000 hospitals and 10,000 other types of healthcare facilities. All accreditors serve the same function of inspection and accreditation of quality in health facilities to assure CMS that the health care provided meets or exceeds conditions of payment for services participation set by the federal government. This allows the approved health provider to receive payments and other monies from Medicare and Medicaid.
Please remember that although accrediting organizations are a vital link between tax dollars and health care, these organizations are not part of the federal government. They are independent contractors serving the function of assuring federal and state authorities and, in turn, private insurers and citizens that each healthcare facility they accredit provides an elevated level of quality care. The approval process is often referred to as the health services provider gaining a “deemed” status, as in deemed worthy to receive payments. This course will focus on The Joint Commission National Patient Safety Goals as annual training requirements due to TJC’s size, standing, close working relationship with CMS, and the history of comprehensive observation and inspection of its expectations.
| Goal | Patient Identification |
|---|---|
| NPSG.01.01.01 | |
| Goal | Improve Communication |
| NPSG.02.03.01 | Improve the effectiveness of communication among caregivers. Report critical results of tests and diagnostic procedures on a timely basis. |
| Goal | Medication Safety |
| NPSG.03.04.01 | Label all medications, containers, and other solutions on and off the sterile field in perioperative and other procedural settings. |
| NPSG.03.05.01 | Reduce the likelihood of patient harm associated with the use of anticoagulant therapy. |
| NPSG.03.06.01 | Maintain and communicate accurate patient medication information. |
| Goal | Clinical Alarm Safety |
| NPSG.06.01.01 | Improve the safety of clinical alarm systems. Make improvements to ensure that alarms on medical equipment are heard and responded to on time. |
| Goal | Health Care-Associated Infections |
| NPSG.07.01.01 | |
| Goal | Improve Health Care Equity |
| NPSG.16.01.01 | Improving healthcare equity is both a quality and safety priority. Identify health care disparities in the patient population and provide a written plan describing ways to improve health care equity. |
| Goal | Identify Patient Safety Risks |
| NPSG.15.01.01 | |
| Goal | Prevent Mistakes in Surgery |
| UP.01.01.01 | Make sure the correct surgery is done on the correct patient and at the proper place on the patient’s body. |
| UP.01.02.01 | Before the procedure, mark the correct place on the patient’s body where the surgery is to be done. |
| UP.01.03.01 | Pause before the surgery to ensure a mistake is not being made. |
| Goal | Prevent Falls |
| NPSG.09.02.01 | Find which patients are most likely to fall—for example, taking medicines that might make them weak, dizzy, or sleepy. Take action to prevent falls for these patients. |
| Goal | Prevent Bed Sores |
| NPSG.14.01.01 | Find which patients are most likely to develop bed sores. Take action to prevent bed sores in these patients. Set times to re-check patients for bed sores. |
(JCR Staff, 2024f; TJC, 2024a)
The Joint Commission's national patient safety goals clearly map which areas will be the target of interest and inspection during accreditation surveys or inquiries. Be sure to address the topics found in the TJC safety goals in your annual training. Joint Commission surveyors will be checking for NPSG training.
Communication between health professionals and accrediting bodies is meant to flow both ways. Should you have concerns about client safety or quality of care, both CMS and Joint Commission have avenues of communication open to hear your questions and concerns.
Recognizing and Reporting Abuse
All clients should be screened for abuse. Facilities must have procedures for identifying, reporting, and treating victims of abuse. Clients have the right to expect access to protective services in the case of abuse.
| Agency Regulation | Ongoing Required Training |
|---|---|
| CMS 482.13(c)(3) | During its orientation and ongoing training programs, the hospital provides ALL employees with information regarding abuse and neglect and related reporting requirements, including prevention, intervention, and detection. |
(CMS, 2023a)
Abuse can take many forms. It may include emotional abuse, economic abuse, sexual abuse, threats, the threat of removing children, using privilege, intimidation, isolation, and other behaviors used to maintain fear, intimidation, and power. There are many theories as to why some people are abusers. However, the reason abusers use this behavior is that violence is an effective method for gaining and keeping control over another person.
Sexual abuse is an unwanted sexual activity with perpetrators using force, making threats, or taking advantage of victims who are not able to give consent. Most victims and perpetrators know each other. Immediate reactions to sexual abuse include shock, fear, or disbelief. Long-term symptoms include anxiety, fear, or post-traumatic stress disorder. While efforts to treat sex offenders remain unpromising, psychological interventions for survivors, especially group therapy, appear effective.
Psychological abuse occurs when a person tries to control information available to another person with the intent to manipulate that person’s sense of reality or their view of what is acceptable and unacceptable. Psychological abuse often contains strong, emotionally manipulative content and threats designed to force the victim to comply with the abuser’s wishes. It can include constant verbal abuse, harassment, excessive possessiveness, isolating the person from friends and family, deprivation of physical and economic resources, and destruction of personal property.
Physical abuse is physical force or violence that results in bodily injury, pain, or impairment. It includes assault, battery, and inappropriate restraint. It often begins with what may be excused as trivial contact that escalates into more severe and frequent attacks.
Use of Restraints
Sometimes, clients need to be kept safe from their own actions. While we always encourage individuals to exercise internal control, at times, there may be a need for external measures of restraint. The decision to use physical or chemical restraints is a medical decision. Restraints must never be used for discipline or convenience. When a client requires external restraint, protecting that person’s safety, rights, comfort, and dignity is important.
| Agency Regulation | Ongoing Required Training |
|---|---|
| CMS 483.13(e) (10-11) CMS 482.13(f) |
Periodic ongoing restraint and seclusion policy training for any staff involved in the process |
| TJC PC 03.05.17 EP.2,4,5 | Qualifications, education, and training for staff allowed to initiate restraint or seclusion and perform 15-minute assessments of patients in restraint or seclusion. Demonstration of staff competence to perform these duties |
(CMS, 2023a; JCR Staff, 2024c)
Review the equipment, policies, and documentation tools for each facility where you practice, as there may be some variation in practice and definition of restraints. Restraint standards for medical/surgical purposes apply when the primary reason for use directly supports medical healing. Please note that slightly different standards are used for behavioral management, such as in a psychiatric setting and long-term care (JCR Staff, 2024c).
Medical vs. Behavioral Restraint Use
In past years, the Joint Commission has differentiated between physical and chemical restraints used for safety in medical settings and physical or chemical restraints used in mental health or behavioral treatment settings. That separation still exists yet is diminishing.
Behavioral use of restraints is a last-used option and should be considered only when a client is imminently at risk of harming themselves or others with their behaviors. Less intrusive methods of regaining safety must be attempted before restraint is applied.
Medication to control behavior should be used only as part of a therapeutic plan after appropriate assessment by professionals. Chemical restraint is a term used to describe using medications for purposes unrelated to the client’s medical condition. An example is the use of a sedating psychotropic drug to manage or control behavior.
It is the intended use of a device that classifies the device or method as a restraint. For instance, IV arm-boards, postural support devices, orthopedic appliances, and protective devices like helmets are not restraints when used to promote healing or protect an easily injured tissue or surgical site.
| According to The Joint Commission, A bed enclosure or side rails are neither purely a restraint nor a form of seclusion, based on the definitions that accompany the Joint Commission standards. However, a bed enclosure (e.g., net bed) and, likewise, a side rail could potentially restrict a patient's freedom to leave the bed and, as such, would be a restraint. If, for example, a bed rail is used to facilitate mobility in and out of bed, it is not a restraint. It would not be a restraint if the patient/client could release or remove the device. |
(TJC, 2022)
Restraints or seclusion are to be used as a last resort after all alternatives have proven unsuccessful. Restraints should not cause harm or be used as a form of punishment. Examples of other options for restraints include but are not limited to.
- Interaction on a 1:1 basis with staff.
- Redirection.
- PRN medication with client consent.
- Staff or client-initiated time out in a quiet room with the door unlocked. It should be presented as a way for a client to regain control, not as a threat.
- Staff presentation of limits where consequences are presented for the client to choose from.
- Removal of stimuli from the client or vice versa. Remember that moving a client close to a busy nurses' station so you can keep a close eye on them could overstimulate and worsen symptoms.
- Relaxation exercises.
- Calming music.
- Distraction tactics.
If lesser interventions are unsuccessful, and you must apply physical restraint as a last resort, use the least restrictive device possible. For example, a lap buddy is a soft vinyl device that attaches to the wheelchair rather than the client. Although the client can remove it when they are oriented, it serves as a reminder that they should not get up without assistance and protects them if they become confused again. Another alternative is a geriatric chair set in a reclining position or with a lapboard. This is less restrictive than a safety belt or roll belt. A roll belt, in turn, is less restrictive than a vest restraint. Mitts are more suitable than wrist restraints because they are less restrictive and allow clients to move their arms freely. Another option is elbow restraints, which keep the arm straight but allow free movement.
A licensed, independent practitioner must order the restraint or seclusion; however, the facility may authorize qualified staff members, usually registered nurses, to initiate the use of restraints when needed before an order is obtained. The independent practitioner must evaluate the need for restraint or seclusion and assess the client within 1 hour.
The authorized staff member can discontinue restraints or seclusion when the assessment reveals that restraints or seclusion are no longer necessary. Restraints for acute medical or surgical purposes must be reviewed and renewed if needed by the licensed, independent practitioner at least every 24 hours. The use of restraints for behavioral healthcare purposes in long-term care must be reviewed and renewed if needed by the licensed, independent practitioner at least every 30 days.
Procedures for checking and documenting while a client is in restraints are rigorous. Each facility will have a restraint or seclusion documentation tool that must be completed, including the following.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC PC.03.05.13 | |
| TJC CTS.05.06.03 | Ongoing education and continuous assessment of staff competence. |
(JCR Staff, 2024c)
The written order in the chart must include the justification for restraint or seclusion, the type of restraint used, and the time limit for use. Some facilities will have a template for the physician’s order. The documentation of restraints and seclusion needs to include the circumstances that led to seclusion or restraint, consideration or failure of non-physical interventions, rationale for intervention used, notification of family if appropriate, criteria for discontinuation as well as informing the client of the behavior criteria, each evaluation, any assistance provided to the client, continuous monitoring, debriefing of client with staff and any injuries that are sustained and treatment received.
Physical restraints should always be fastened for easy release in an emergency. The restraint should be attached to a fixed part of the furniture, like the bed frame. Fixing it to a movable part, like a side rail, could inadvertently tighten the restraint, causing client injury, or could loosen the restraint, causing it to be ineffective.
| A Joint Commission surveyor comes to the ward where a client is in behavioral restraint due to an assault and secluded in a corner room due to her loud cursing and continuous verbal threats upsetting other clients. The primary physician is awaiting drug toxicology results before beginning a medication process to calm the client, and a staff member is sitting at the foot of the clients’ bed, observing their vital signs and respiration. The surveyor asks the observing staff if she can speak to them at the nurse’s station away from the anxious, animated client. The observing staff refuses, stating that this client must always have continuous, direct attendance. What reaction do you anticipate from survey personnel spurned? |
This is a WIN! No person in seclusion AND restraint can be left alone at any time, for any reason. The possibilities of things going wrong while in restraints and isolation are overwhelming; here are a few.
|
Fall Reduction
A high fall risk is not an acceptable reason to use restraints. The following are suggestions to reduce fall risk:
- Check the client at least every hour.
- Remind the client to call for assistance if they want to visit the bathroom.
- Use low beds or put the mattress on the floor for high-risk clients who will not call for assistance to get up.
- Arrange furniture so that it does not block the walkways.
- Use nightlights and keep debris and liquids off the floor.
- Always keep the client's personal items, water pitchers, and call light within reach.
- Make sure the client wears their eyeglasses, hearing aids, or other assistive devices.
- Ask family or friends to stay with them at night or when they will likely try climbing out of bed.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC HR.01.05.03 | Ongoing education and training on fall reduction. |
(TJC, 2024a)
Violence Preparation
PBS News reports (Yang,2023) that the risk of violence to healthcare workers is much higher than for all other private sector industries. Documentation clearly shows that 73 percent of all non-fatal injuries from violence occur to healthcare professionals.
The circumstances of hospital violence differ from workplace violence in other settings, such as banks, convenience stores, or taxicabs, where violence most often relates to robbery. Violence in hospitals is usually an outpouring of emotion rather than an attempt at material gain, with violence toward others resulting from clients or their family members who feel frustrated, vulnerable, and out of control. Common risk factors for hospital violence include the following.
- Working directly with volatile people, especially if they are under the influence of drugs or alcohol or have a history of violence or certain psychotic diagnoses.
- Working when understaffed-especially during mealtimes and visiting hours.
- Transporting clients.
- Long waits for service.
- Overcrowded, uncomfortable waiting rooms.
- Working alone.
- Poor environmental design.
- Inadequate security.
- Lack of staff training and policies for preventing and managing crises with potentially volatile patients.
- Drug and alcohol abuse.
- Unrestricted movement of the public.
- Poorly lit corridors, rooms, parking lots, and other areas.
Violence may occur anywhere in a hospital but is most frequent in psychiatric wards, emergency rooms, waiting rooms, and geriatric units. Studies indicate that violence often takes place during times of high activity and during interaction with clients. Assaults may occur when service is denied, when a client is involuntarily admitted, or when a healthcare worker attempts to set limits on eating, drinking, tobacco, or alcohol use. Clients with any condition that causes confusion and impaired judgment are more likely to become violent than clients with normal mentation. Neurologic conditions, seizures, hypoglycemia, or dementia may cause confusion and impaired judgment. Watch for signals that may be associated with impending violence.
- Verbally expressed anger and frustration.
- Body language such as threatening gestures.
- Signs of drug or alcohol use.
Also, it is important to note how your co-workers behave. If a colleague’s demeanor or behavior has worsened, notify your manager. For example, slamming equipment around is red-flag behavior.
Learn from history. If a client has a history of violent behavior (such as acting combative in the ambulance or waiting room), prepare yourself for potentially violent behavior and warn others who are caring for them. Let security know if you feel threatened or if you find or suspect that he is carrying a weapon. Notify the supervisor if you suspect a client is going to be violent. Help relieve the client’s tension and anxiety by informing him about when he will be examined or treated and what is happening.
Be alert to your environment.
- Evaluate each situation for potential violence when you enter a room or begin to relate to a patient or visitor.
- Be vigilant throughout the encounter.
- Do not isolate yourself from a potentially violent person.
- Plan your exit. Always keep an open path for exiting. Do not let the potentially violent person stand between you and the door.
- When you are with an upset client or co-worker, avoid areas of the room that lack an accessible exit.
- If you go to an isolated part of your facility, let others know where you are going and when you expect to return.
- Consider asking for an escort.
- Note that anyone not wearing staff ID is lingering where they should not. Politely ask if you can help them and notify security if you are unsatisfied with the answer. Call security and provide a complete description if you would rather not approach someone.
- Evaluate how you wear equipment to be sure it cannot be used as a weapon against you. For example, consider that a stethoscope or ID badge without a breakaway necklace can be used to choke you. Carry your stethoscope in a pocket and use an ID badge necklace with a breakaway feature.
- If you wear a necktie, opt for a clip-on style.
- If your hair is long, wear it in a way that is not easy to pull, and do not wear dangling jewelry.
In the presence of a potentially violent person:
Do
- Plan a clear exit route.
- Keep 5 to 7 feet between you and him. Never turn your back on him or let him get between you and the exit.
- Keep your voice calm and quiet.
- Acknowledge that he has a right to his feelings.
- Assume that he has a valid concern and address it.
- Try to meet reasonable demands.
- Offer alternatives when possible. For example, tell an angry patient that although he cannot order take-out pizza, you will see if you can get him an early dinner. Tell an angry colleague that you see that she is angry and that you would like to work with her and your manager to resolve the situation.
- Call for backup or security if a situation grows increasingly tense.
- Ensure access to bathrooms, a phone, a TV, and something to read.
- Track equipment. Please return it to its rightful place. When you take an item into a client’s room, dispose of it properly or bring it when you leave.
Take these steps if you cannot defuse the situation quickly:
- Remove yourself from the situation.
- Call security for help.
- Report any violent incidents to your management.
Do not!
- Do not ignore the agitated person or avoid him.
- Do not threaten or demand obedience.
- Do not argue or become defensive or judgmental.
- Do not laugh, move suddenly, make threatening gestures, or invade his personal space.
- Do not try to manage a dangerous situation alone. Call security or initiate your facility’s violence prevention protocol.
In the presence of a weapon, maintain behavior that helps diffuse anger:
- Present a calm, caring attitude.
- Do not match the threats.
- Do not give orders.
- Acknowledge the person’s feelings (for example, “I know you are frustrated”).
- Avoid any behavior that could be interpreted as aggressive (for example, moving rapidly, getting too close, touching, or speaking loudly).
Sexual Harassment
Let us face it: something about the healthcare environment brings out the best and the worst in people and their behaviors. Sexual harassment is not acceptable and can lead to civil prosecution and disciplinary action up to termination. Sexual harassment includes unwelcome:
- Sexual advances.
- Request for sexual favors.
- Verbal, visual, or physical behavior of a sexual nature.
State laws and requirements control the mandate for training concerning preventing sexual harassment in the workplace. Be assured that training will be required for ALL employees on a frequency specific to your state laws. National oversight of sexual harassment policies and complaints is provided by the U.S. Office of Civil Rights (OCR), and they are proactive in exerting authority when incidents are reported (OPA, 2024).
Sexual harassment becomes unlawful when it becomes a condition of employment or advancement, unreasonably interferes with work performance, or creates an intimidating, hostile, or offensive work environment.
| Agency Regulation | Ongoing Required Training |
|---|---|
| OCR Title VII | Training is strongly recommended by the U.S. Equal Employment Opportunity Commission (EEOC). The EEOC guidelines apply to employers in all states, and |
(Krofcheck, 2023)
Work environments vary, and people have varying levels of sensitivity. The worker is responsible for informing the people involved to stop because they are offended or feel sexually harassed. If the behavior continues, report it to your supervisor or the human resources department. Do not mistakenly think it will go away on its own. Like a lingering foul stench, harassment requires positive action to have it cease.
Radiation Safety
The primary sources of radiation exposure in a healthcare facility are X-rays and radionuclides used in diagnostic tests and therapy. Areas where radiation is used are marked with the international tri-foil symbol.
 Ionizing Radiation |
 Non-ionizing radiation |
|
|
(OSHA, 2023b)
Remember, portable X-ray machines might be tucked in closets, storage rooms, at the side hall of emergency or critical care units, or in many other unmarked areas.
| Agency Regulation | Annual Required Training |
|---|---|
(N.C. Department of Labor, 2022)
During radiation exposure, you should limit your time as much as possible, move at least six to ten feet from the source, and wear lead shields. If your job requires routine exposure, you should wear a monitoring device to measure your exposure. When working with radioactive material, wash your hands thoroughly and properly dispose of trash. Do not eat, drink, smoke, or apply products to your skin in an area where radioactive material is being used.
Environment Safety
For most health professionals and every organization in the health industry, the major regulatory authorities expecting targeted annual training are TJC, CMS, and OSHA. Let us look at training topics that focus on safety in the workplace from the perspective of those organizations’ expectations.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC EC.03.01.01 EP.1 CMS 482.41 (b)(1)(i) |
Ongoing training so staff knows how to identify physical risks in the care environment and demonstrate how to eliminate them. |
| TJC EC.03.01.01 EP.2 CMS 482.41 (b)(1)(i) |
Ongoing training so staff can demonstrate the ability to handle an environment of care incident. |
(JCR Staff, 2024g)
Ergonomics
Back injury prevention, safe lifting, and safe movements fall under ergonomics. Ergonomics is a science that designs equipment and work tasks to fit the worker. The goal is to prevent worker injury. If you have pain, tingling, or numbness associated with a specific activity, reevaluate how you perform the task to ensure you do it correctly. Consult your supervisor or employee health provider for an ergonomic evaluation of your work. There may be equipment and methods available to reduce the risk of injury.
| Agency Regulation | Ongoing Required Training |
|
The rules around OSHA ergonomics training are tricky. Currently, there are no direct federal regulations mandating ergonomics training for employees. However, OSHA mandates for safe and healthy work practices include interpretations that might as well be entitled ergonomics. This means that in practice, since 2001, OSHA ergonomic-focused rules apply to all general industries, including workers involved with healthcare.
|
|
(OSHA, 2023b)
Injuries and illnesses that affect muscles, nerves, tendons, ligaments, joints, or spinal discs are known as musculoskeletal disorders (MSDs). Injuries can result from cumulative trauma and repetitive strain, where small injuries, over time, build up until one more injury triggers a debilitating MSD. The following tasks have a substantial risk of cumulative trauma and repetitive strain:
- Repetitive activity (typing).
- Contact stress (hammering).
- Twisting while lifting or carrying.
- Pulling or dragging.
- Sitting or standing in one position for a long time.
- Reaching above your shoulder.
- Lifting.
- While stooping low.
- Heavy objects.
- Unwieldy objects.
- Reaching for or using an object positioned far from your body.
- Frequent lifting without rest between lifts.
The primary approach to preventing back injury involves reducing manual lifting and other load-handling tasks that are biomechanically stressful. The secondary approach is to train workers to perform stressful tasks while minimizing the biomechanical forces on their backs, maintaining flexibility, and strengthening the back and abdominal muscles. To prevent back injury, workers should:
- Use tools to avoid lifting when possible.
- Lifting devices.
- Slide boards.
- Shower chairs.
- Gait belts.
- Use proper lifting techniques.
- Keep your back in its normal upright position when lifting.
- Keep your head and shoulders up and tighten your abdominal muscles when lifting.
- Bend at the knees, not at the waist.
- Get a good grip and slightly bend your elbows.
- Lift with your legs in a smooth, even motion, not with your back.
- Bear the weight with your arms and legs, not your back.
- Bear the weight as close to your body as possible.
- Pivot on your feet to change direction; do not twist.
- Lower an object by widening your stance and bending your knees.
- Do not reach higher than your shoulders to lift.
- Limit the number of lifts per day.
- Request help. When in doubt about whether a task may strain the back, a worker should request help rather than take a chance.
- Back exercises can strengthen the back muscles and help prevent back injuries. A physician or physical therapist should be consulted.
- The benefit of using back belts is undetermined. The belt may lead to a false sense of security and a failure to use proper lifting techniques. This can lead to injuries.
Client transfers are particularly hazardous for healthcare professionals. The following special points should be emphasized to prevent back injuries during transfers (Atwell, 2023).
- Obtain lifting equipment as applicable.
- Do not do a manual transfer alone.
- Position equipment and furniture effectively (for example, move a wheelchair beside the bed) and remove obstacles.
- Communicate the action plan to the client and other workers to ensure the transfer is smooth without sudden, unexpected moves.
- Use a wide, balanced stance.
- Ensure sound footing for the client if applicable (clients should wear slippers that provide good traction).
- Maintain eye contact and communication with the client. Be alert for trouble signs.
- Record any problems on the client’s chart so that other workers will know how to cope with difficult transfers. Note the need for any special equipment, such as a lift.
Injury Prevention
If you are injured or exposed to a dangerous substance on the job, stop what you are doing; report the injury or exposure to your supervisor; seek medical attention if needed; and complete an employee accident report.
| Agency Regulation | Ongoing Required Training |
|---|---|
| OSHA 29.CFR.1910.1200 | Initial and ongoing training (annual recommended yet not articulated in the guideline) on Hazard Communication to increase workplace safety. |
(N.C. Department of Labor, 2022)
Accident hazards such as wet floors, stairway obstructions, and faulty ladders make the environment of care dangerous; eliminate them. Wet-floor hazards can be reduced by proper housekeeping procedures such as marking wet areas, cleaning up spills immediately, cleaning only one side of a passageway at a time, keeping halls and stairways clear, and providing good lighting for all halls and stairwells. Stairway hazards can be minimized by using the handrail on stairs, avoiding undue speed, and maintaining an unobstructed view of the stairs ahead, even if that means requesting help to manage a bulky load.
Chemical Hazards
All healthcare facilities are required to have
| Agency Regulation | Annual Required Training |
|---|---|
| OSHA 29.CFR.1910.1200 | Annual Hazard Communication Training. |
(N.C. Department of Labor, 2022)
Product identification.
Hazard(s) identification.
Composition/ information on ingredients.
First-aid measures.
Fire-fighting measures.
Accidental release measures.
Handling and storage.
Exposure controls/personal protection.
Physical and chemical properties.
Stability and reactivity.
Toxicological information.
Ecological impact information (Non-mandatory).
Disposal considerations (Non-mandatory).
Transport information (Non-mandatory).
Regulatory information (Non-mandatory).
Other information, including the date of preparation or last revision of the SDS or the last change to it.
Chemicals may exert either acute or chronic effects on workers. The effects depend on the following:
- Extent (concentration and duration) of exposure.
- Route of exposure.
- Physical and chemical properties of the substance.
Did you know that all the hazard pictograms used in the United States have already been replaced with international symbols? That was a nationwide training mandate for 2013, and you had better be on guard for questions related to the new SDS and hazard symbols during surveys.
The new worldwide visual warning system is part of the Globally Harmonized System of Classification and Labeling of Chemicals (GHS) and uses two sets of warning pictograms. One set is for transporting chemicals, and the second is for workplace use and storage.
Let us look at a new pair of warning symbols that have replaced the retired poison pictogram commonly found in medical closets and work areas.
| Health Hazard | Skull and Crossbones |
|---|---|
 |
 |
|
|
Effects exerted by a substance may also be influenced by other chemicals and physical agents or by an individual’s use of tobacco, alcohol, or drugs. The exposure dose is the amount of a substance that enters the body during exposure. The substance continues to be present in the body until it is metabolized or eliminated. Although some chemicals are rapidly metabolized, others are not and may be excreted unchanged or stored in the fatty tissues (solvents), lungs (dust and fibers), bone (lead and radium), or blood (soluble gases).
| Agency Regulation | Annual Required Training |
|---|---|
| OSHA 29.CFR.1910.1001(j)(7) | Annual Airborne Asbestos Training |
| OSHA 29.CFR.1910.120(e) OSHA 29.CFR.1910.120. App C |
Annual Hazardous Waste Training Annual Hazardous Waste Emergency Response Training |
| OSHA 29.CFR.1910.1045(o)(1) | Annual Hazardous Substance Training – Acrylonitrile |
| OSHA 29.CFR.1910.1028(j)(1) | Annual Hazardous Substance Training – Benzene |
| OSHA 29.CFR.1910.1003(e) | Annual Hazardous Substance Training – Carcinogens |
| OSHA 29.CFR.1910.1047(j)(3) | Annual Hazardous Substance Training – Ethylene Oxide |
| OSHA 29.CFR.1910.1048(n)(1) | Annual Hazardous Substance Training – Formaldehyde |
(N.C. Department of Labor, 2022)
Toxic substances can enter the body through several routes, including intact skin, the respiratory system (inhalation), the mouth (inhalation and ingestion), the eyes, and by accidental needle punctures. Inhalation and skin exposure are the most likely. Some substances can also damage the skin or eyes directly without being absorbed. Not all substances can enter the body through all routes. Inorganic lead, for example, can be inhaled or swallowed, but it does not penetrate the skin. Exposure routes for antineoplastic and other hazardous drugs are inhalation, skin absorption, ingestion, and injection.
Not every toxic substance’s annual training requirement should be on your individual training list. It would be best if you were not handling asbestos, for instance. However, someone in the hospital or at the care site does, as many buildings used for offices, clinics, and hospitals fall into the period during which asbestos was used in flooring, ceiling products, building insulation, and many other practical products. Take the time to find out which specific substances are used and managed in your work setting and whether you need any of the annual training concerning them.
Fire Prevention
Training in fire safety is not only required by the major regulatory agencies; it is common sense. Any health professional who has lived through a fire in a care setting knows and has night terrors about the complexity of moving ill clients out of harm’s way in an emergency.
OSHA, the Occupational Safety and Health Administration, and NFPA, the National Fire Protection Association, both have strong guidance on healthcare facility safety. Point of trivia: when CMS surveyors investigate an organization’s physical safety and disaster planning, they pull out the NFPA guidelines and go by them. To satisfy CMS, know, follow, and exceed NFPA guidelines.
| Agency Regulation | Annual Required Training |
|---|---|
| TJC EC.02.03.03 | Annual Fire Drill Training |
| OSHA 1910.156(c)(2) | Annual Fire Brigade Training |
| OSHA 1910.157(g)(2,4) | Annual Portable Fire Extinguisher Training |
| OSHA 1910.158(b)(10) | Annual Fixed Fire Extinguisher Training |
(JCR Staff, 2024h; N.C. Department of Labor, 2022)
In healthcare, we are all expected to render assistance during situations that place our clients at risk. We, therefore, all require a working understanding of fire response, small fire suppression, and tactics to slow the spread of larger fires. As found in OSHA regulations, a fire brigade designation does not pertain to every health worker but to those who have received additional fire suppression and rescue instruction. If you have the floor or unit staff designated as “safety officers” or “fire wardens,” please review the OSHA Fire Brigade definitions to ensure they receive correct training before an inspection or cross your fingers before you are called to perform in an emergency.
| Agency Regulation | Ongoing Required Training |
|---|---|
| NFPA 16.14.3.10.2 NFPA 16.14.3.10.3 |
Continuing safety education and supervision shall be provided for Operating Room staff (and others), incidents shall be reviewed monthly, and procedures shall be reviewed annually. Fire exit drills shall be conducted annually or more frequently as the applicable code determines. |
(JCR Staff, 2024e; NFPA, n.d.)
For all of us, when you enter a new work area, look around and find fire alarms, fire extinguishers, exit signs, and oxygen cut-off valves. One way to remember fire safety is the acronym RACE.
- R: rescue
- A: alarm
- C: contain the fire (if possible)
- E: extinguish or evacuate
Never hesitate to sound the alarm with any suspicion of fire, yet never “fire.” Yelling “fire” creates panic. Instead, call out the facility's verbal code for fire. Call the switchboard to report the fire and pull the fire alarm. When you call the switchboard, please stay on the phone long enough to ensure they have received the correct information, such as where you are!
If a fire is small and confined, you may be able to extinguish it. If a client’s garments are on fire, wrap them tightly in a large blanket to extinguish the flames. If a piece of equipment catches fire, pull the plug or cut the electricity as soon as possible.
OSHA is clear if you place hand-held portable fire extinguishers for staff to use in emergencies, you must train every staff member annually on how to use them. Portable fire extinguishers come in different classes for use on fires of diverse sources. The extinguisher has small pictures on the label that help you identify the type of fire source material they should be used on. Class A puts out fires involving ordinary combustibles. Class B extinguishers smother fires involving flammable liquids or gases. Class C extinguishers put out fires in or near electrical equipment. Type ABC extinguishers can be used to fight all three types of fires.
To use an extinguisher, remember PASS:
- Pull the pin
- Aim the nozzle at the base of the fire
- Squeeze the trigger while making
- Sweeping strokes with the extinguisher plume
If a fire cannot be extinguished and smoke, fumes, or flames threaten client safety, you may need to evacuate. Evacuate ambulatory clients first. Stay calm and give clear directions. Evacuate horizontally for as long as you can. Then, evaluate vertically down to a lower level. Never use an elevator to escape during a fire. A sudden loss of power could leave you and your client trapped inside the elevator.
Healthcare units are required to be separated by heavy fire doors that close automatically when the alarm is sounded to keep the fire from spreading. To confine a fire, close the doors, windows, and all vertical openings like the laundry chute. Stuff wet towels under the doors to keep smoke out. Shut off oxygen supplies if directed to do so. Usually, facility policy designates someone in supervision to decide when to turn off oxygen supplies.
When rescuing anyone in immediate danger, remember to stay low. Smoke rises to the ceiling, forming a heavy, dense cloud that slowly descends. This cloud is deadly because it contains toxic gases.
Staff responsible for inspecting, maintaining, or repairing fixed fire extinguishing equipment such as sprinklers or fire hose reels must be trained annually concerning these essential safety items.
Emergency Management Disaster Preparedness
Katrina, Joplin, Missouri, the Twin Towers; the list of disasters affecting hospitals, all of us in the health professions, is limitless since emergencies come to us, either physically or by proxy, in the form of waves of injured.
| Agency Regulation | Annual Required Training |
|---|---|
| TJC EC.03.01.01 | Annual Emergency Response Training |
| OSHA 29.CFR.1910.120(q) | Annual Emergency Response Training |
| CMS 40.CFR.311 | Annual Emergency Response Training |
| NFPA 99 | Incident command and emergency management department- and staff-specific education shall be conducted upon appointment to department/staff assignments or positions and annually after that. |
| CIHQ EP-5 (D) | Emergency preparedness training should be provided to all staff, individuals providing services under contract arrangement, and volunteers at least every two years to ensure their expected role is met. |
(CIHQ, 2024; CMS, 2023b; JCR Staff, 2024g; N.C. Department of Labor, 2022; NFPA, n.d.)
Joint Commission requests and requires annual training for emergency responses specific to healthcare facilities, including twice-yearly live emergency scenarios (e.g., bomb threat, hostage situation, facility fire, plane crash into the building, etc.). At least one of these annual training must involve the community around the organization, such as the fire department, search and rescue, police, etc. Be aware that TJC requires an assigned survey member at these exercises to monitor performance and document deficiencies, with staff training following up to correct anything found lacking. Do not be tempted to take emergency response training lightly; not only will regulatory agencies grade it, but it could also save the lives of those precious to you.
Supervisors must know how to initiate the disaster plan and designate worker tasks.
Each worker must be trained to:
Locate the disaster plan on each unit where they work. Know the alarm codes for each type of disaster. Know the exit routes. Know how to use any evacuation equipment.
Alarm System
As of January 1, 2016, the Joint Commission began expecting ongoing training on the purpose and correct operation of medical device alarm systems. This is now an expectation for every healthcare professional using any device with alarms.
| Agency Regulation | Annual Required Training |
|---|---|
| TJC NPSG.06.01.01 | Purpose and Correct Operation of Alarm Systems |
(JCR Staff, 2024f)
Every medical device possesses an audible or visual alarm these days, and the wild cacophony that is heard and often ignored in health settings is a cause of “alarm fatigue” to both the public and regulatory agencies. Knowing when to set the alarm, how to set it, and how to respond promptly requires proper training and accountability.
As health systems move further into the age of electronic health records and systems, expect digital monitoring of essential medical equipment. In other words, should equipment alarms sound consistent without being addressed, the marvelous mechanism of the Joint Commission Tracer System is likely to stumble upon and take notice. So, train appropriately, staff accordingly, work intelligently, or practice how to respond to accreditation surveyor queries.
Infection Prevention
Every health professional knows the drill: Infection = Bad, Prevention = Good. It is a shame that it is not that easy, with new organisms and changing drug resistances always cropping up. CMS, Joint Commission, OSHA, and every state have expectations concerning the annual training of health workers on infection prevention and failing infection control.
| Agency Regulation | Annual Required Training |
|---|---|
| TJC NPSG.07.03.01 EP.2 | Healthcare-associated infections, multidrug-resistant organisms, and prevention strategies. |
| TJC NPSG.07.04.01 EP.1 | Central line-associated bloodstream infections and the importance of their prevention. |
| TJC NPSG.07.05.01 EP.1 | Surgical site infections and the importance of their prevention. |
| OSHA 29 CFR 1910.1030(g)(2) | Bloodborne Pathogens Annual Training. |
| CMS 482.42 | Ongoing infection prevention training for all staff. |
(Chambers, 2023; JCR Staff, 2024f)
Hand Washing Guidelines
Under the current Centers for Disease Control (CDC) handwashing guidelines, washing hands with soap and water is to be done whenever the hands are visibly dirty.
- Client contact.
- Donning gloves when inserting a central venous catheter (CVC).
- Inserting urinary catheters, peripheral vascular catheters, or other invasive devices that do not require surgery.
Hand hygiene is also indicated after:
- Contact with a client’s intact skin.
- Contact with body fluids, excretions, non-intact skin, or wound dressings.
- After removing gloves.

Efficacy of Hand Hygiene Material
Standard Precautions
Standard precautions are strategies for protecting healthcare workers from the occupational transmission of organisms. The premise is that all pre-existing client infections cannot be identified; therefore, barrier precautions should be used routinely to protect from all sources of potential infection. Standard precautions apply to blood and all body fluids, secretions, and excretions except sweat, regardless of whether they contain visible blood, non-intact skin, and mucous membranes. Additional precautions are based on highly transmissible or epidemiologically important pathogens. Transmission Based Precautions (isolation) are airborne, droplet, and contact.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC IC.01.05.01 TJC IC.02.01.01 |
Training and education on responsibilities related to preventing and controlling infections. |
| CMS 482.23(c)(1) | Ongoing training and competency for administration of drugs and biologicals. |
(CMS Staff 2023a; JCR Staff, 2024i)
Personal Protective Equipment (PPE)
| Agency Regulation | Ongoing Required Training |
|---|---|
| OSHA 1910.132 (f)(1)(i-v);(2),(3)(i-iii);(4) | PPE training is ongoing and as needed. |
(Safety Culture Contact Team, 2024)
Masks, goggles, or face shields should be used to protect the mucous membranes of the eyes, nose, and mouth when there is a likelihood of splashes or sprays. Healthcare workers wear surgical masks to protect against large-particle droplets during close client contact. When tuberculosis is known or suspected, healthcare workers should wear an N95 respirator, a high-efficiency particulate air (HEPA) filter respirator, or a powered air-purifying respirator (PAPR).
Gowns are worn to prevent clothing contamination and protect the healthcare worker’s skin from exposure to blood and body fluids. Impermeable gowns, leg coverings, boots, or shoe covers provide more protection when copious quantities of blood or body fluids may be splashed. Gowns are also worn as a part of some transmission-based precautions. Mouthpieces, resuscitation bags, or other ventilation devices should be used instead of mouth-to-mouth resuscitation.
Needlestick Prevention
Needles should never be recapped, bent, broken, or removed from contaminated syringes. Sharps should be disposed of in a puncture-proof container and transported to a reprocessing area. Improved engineering controls are among the most effective approaches to reducing occupational hazards and, therefore, are a principal element for a needlestick prevention program. Such controls include eliminating unnecessary needles and implementing devices with safety features. Most injuries from hollow bore needles can be prevented with the use of safer sharps devices, and several sources have identified the desirable characteristics of such safety devices. These characteristics include the following:
- The device has no needle.
- Safety features are an integral part of the device.
- The device preferably works passively (i.e., it requires no activation by the user). If the user action is necessary, the safety feature should be engaged with a single-handed technique, allowing the worker's hands to remain behind the exposed sharp.
- The user can easily tell whether the safety feature is activated.
- The safety feature cannot be deactivated and remains protective through disposal.
- The device performs reliably.
- The device is easy to use and practical.
- The device is safe and effective for client care.
Although these characteristics are desirable, some are not feasible, applicable, or available for certain healthcare situations. For example, needles will always be necessary where alternatives for skin penetration are not available. Also, a safety feature that requires activation by the user might be preferable to one that is passive in some cases. Each device must be considered on its merit and ability to reduce workplace injuries. The desirable characteristics listed here should serve only as a guide for device design and selection (OSHA, n.d.)
Transmission-Based Precautions (Isolation)
Transmission-based precautions and protective environment (PE) are terms used to describe protective measures that need to be employed by specific groups of clients. An older term for this was isolation. Clients requiring transmission-based precautions require a private room. Clients infected with the same organism can share a room. This is referred to as cohorting (CDC, n.d.).
Contact Precautions
Contact precautions are used for clients with known or suspected infections or who are colonized with epidemiologically important microorganisms that can be transmitted by direct or indirect contact (CDC, n.d.b). Examples include:
- Presence of stool incontinence (may include norovirus, rotavirus, or Clostridium difficile), draining wounds, uncontrolled secretions, pressure ulcers, or presence of ostomy tubes and bags draining body fluids.
- Presence of generalized rash.
For contact precautions, clients should be in a private room. Standard precautions should be used, and a gown should be worn if direct contact with the client or environmental surfaces is likely.
Airborne Precautions
Airborne precautions are implemented for diseases transmitted by microorganisms in airborne droplet nuclei (CDC, n.d.b). Droplet nuclei are tiny particle residues left when droplets evaporate. Droplet nuclei remain suspended in the air and can be widely dispersed by air currents. Early identification and triage of suspected cases of airborne transmitted diseases should be made, and infectious clients should be separated from others and asked to wear a surgical mask.
Airborne precautions require a specially ventilated room with at least six air changes per hour, negative air pressure relative to the hallway, and outside exhaust or HEPA-filtered recirculation. The door to the room must be kept closed. The negative air pressure should be monitored. An N-95 mask, or a powered air-purifying respirator (PAPR), is used by health workers in airborne precaution settings:
- These masks and respirators should be labeled and stored in a paper bag between uses.
- These masks and respirators should be discarded if soiled or no longer maintain their structural or functional integrity.
- The N-95 mask should also be discarded at the end of each work shift.
- The disposable respirator should be discarded at the end of 2 weeks.
Each employee who may work in an airborne precautions setting must be fit tested to ensure that the N-95 mask or PAPR fits the employee’s face so that droplet nuclei cannot get in gaps between the mask and the face. Be aware employees with beards will not pass fit testing.
When a client in airborne precautions needs to be moved or transported, they should wear a surgical mask from when they leave the isolation room until they return.
Tuberculosis (TB) is a current high-interest topic for training due to nearly (according to WHO, the World Health Organization) 10 million new TB cases every year (CDC, 2024). Estimates that two billion people, one-fourth of the world’s population, may be infected with TB. TB symptoms are cough lasting for more than two weeks, loss of appetite, weight loss, night sweats, hemoptysis, and fever. Clients presenting with these symptoms should be asked to wear a surgical mask until a physician can determine whether to use airborne precautions. If an acid-fast bacillus (AFB) test is ordered, TB is suspected, and airborne precautions should be implemented.
Droplet Precautions
Droplet precautions are used for clients known or suspected to be infected with microorganisms transmitted by droplets generated during coughing, sneezing, talking, or performing procedures (CDC, n.d.b). These microorganisms include, yet are not limited to:
- Respiratory viruses (e.g., influenza, parainfluenza, adenovirus, respiratory syncytial, human metapneumovirus).
- Bordetella pertussis.
- For the first 24 hours of therapy: Neisseria meningitides and group A streptococcus.
Droplet precautions require a private room, but no special ventilation is necessary, and the door may remain open. Masks should be donned upon entering the room, especially if working within three feet of the client. The client should be masked if transported.
Neutropenic Precautions
Neutropenic precautions (reverse isolation) are implemented to protect immunocompromised clients. Neutropenia is a condition that causes low neutrophils in the blood. Neutrophils are a type of white blood cell made in the bone marrow that aids the body in fighting infection. Examples of conditions that might warrant neutropenic precautions include:
- Acquired immunodeficiency syndrome.
- Agranulocytosis.
- Burns, extensive noninfected type.
- Dermatitis, noninfected vesicular, bullous, or eczematous disease (when severe and extensive).
- Immunosuppressive therapy until the patient’s immunity is adequate.
- Lymphomas and leukemia, especially late stages of Hodgkin’s disease or acute leukemia.
Neutropenic precautions require a private room with positive air pressure relative to the air pressure in the hall. Other precautions may range from standard precautions and traffic limitations to extensive precautions using gloves, gowns, and masks. This varies depending on the reason for the precautions and the degree of the client’s immunosuppression.
Central Line and Surgical Infections
Central Line-Associated Bloodstream Infection (CLABSI) and Surgical Site Infection (SSI) prevention are critical areas of concern. Annual training is a focus for any healthcare staff whose job duties place them in contact with central venous catheters (CVCs) or surgical wounds and dressings. CVCs play a vital role in supporting the client, administering intravenous fluids, medications, blood products, and parenteral nutrition, and providing hemodialysis access and hemodynamic monitoring. CVCs have also been identified as one of the most frequent causes of healthcare-related bloodstream infections. SSIs are estimated to account for 20% of all Hospital Acquired Infections (HAIs), leading to longer hospital stays (Canada & Daitch, 2023). It is estimated that this is due to the lack of accurate, voluntary hospital reporting on SSIs. This trend has not gone unnoticed and will inevitably lead to more regulations and oversight should healthcare organizations not be willingly forthcoming concerning important public safety issues.
Infectious Waste Management
In healthcare, everyone is responsible for properly disposing of biohazardous material. One negligent act can result in biohazardous exposure. Biohazard materials include blood and body fluids. If you are in doubt, use a biohazard container to dispose of the material. All biohazardous containers should be red and have the following biohazard symbol.
Biohazard sharps containers are to be red and come in varied sizes.
Biohazardous bags are red and are to be used for biohazardous material that is not sharp and may be contaminated with blood or body fluid. These bags are also used to dispose of chemotherapy drugs and chemicals, even though they are not infectious.

Biohazard Symbol

Biohazard Sharps Container
General waste bags are used for general trash and some body fluids and equipment if there is no visible blood: urine, feces, disposable pads or chux, PPE, used gloves, respiratory care items, and suction canisters. However, if in doubt, use a biohazardous bag.
| Earl from housekeeping is tidying the hematology section of the clinical laboratory at the end of a bustling day. He notices fragments of glass tucked under the counter edge next to the microscopy station. He carefully dons heavy gloves and disposes of the glass shards in the clearly marked sharps container. General cleaning is done; he changes to vinyl gloves for better dexterity and grabs onto a partially filled general-use garbage bag. As he bends his knees to lift, he feels a sharp pain in the palm of his gloved hand, supporting the bottom of the white plastic bag. Grimacing, he looks at his lacerated palm and the sharp jutting dagger of a broken microscope slide poking through the thin material. All sharps, not just needles, go into the designated red sharps container. Anything sharp, such as glass shards, metal fragments, empty vials, blood tubes, microscope slides, glass pipettes, or anything that can become sharp, goes into the sharps box. |
Recommended Healthcare Worker Immunization
Healthcare worker vaccination is a hot-button topic, so anticipate frequent training focused on this topic for years to come.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC IC.02.04.01 EP.2 | Education and training on influenza vaccine, non-vaccine prevention and control, diagnosis, transmission, and impact of influenza. |
(JCR Staff, 2024i)
The CDC’s perspective is that health professionals are always at risk for exposure to serious and sometimes deadly diseases. We each work directly with clients or handle material that could spread infection. Due to these factors, each of us should be appropriately vaccinated to reduce the chance of catching or spreading vaccine-preventable diseases. The CDC hot list of healthcare worker vaccinations includes:
| Hepatitis B |
The absence of documented evidence of a complete hep B vaccine series or an up-to-date blood test (i.e., no serologic evidence of immunity or prior vaccination) warrants a warrant.
|
| Flu (Influenza) | Get one dose of influenza vaccine annually. |
| MMR (Measles, Mumps, & Rubella) | If born in 1957 or later and have not had the MMR vaccine or don't have an up-to-date blood test that shows you are immune to measles or mumps (i.e., no serologic evidence of immunity or prior vaccination), get two doses of MMR (1 dose now and the 2nd dose at least 28 days later). If born in 1957 or later and have not had the MMR vaccine or do not have an up-to-date blood test that shows immunity to rubella, only one dose of MMR is recommended. |
| Varicella (Chickenpox) | If you have not had chickenpox (varicella), if you haven't had varicella vaccine, or if you don't have an up-to-date blood test that shows you are immune to varicella (i.e., no serologic evidence of immunity or prior vaccination) gets two doses of varicella vaccine, four weeks apart. |
| Tdap (Tetanus, Diphtheria, Pertussis) | Get a one-time dose of Tdap as soon as possible if you have not received Tdap previously (regardless of when the previous dose of Td was received). Get Td boosters every ten years after that. Pregnant HCWs need to get a dose of Tdap during each pregnancy. |
| Meningococcal | Those who are routinely exposed to isolates of N. meningitidis should get one dose. |
(Correll, 2023)
Exposure to Bloodborne Pathogens
OSHA possesses a comprehensive bloodborne pathogen standard for workers in areas of risk, including healthcare, housekeeping, and emergency responders, to name a few. As a healthcare professional, be careful to take this topic seriously, as in the U.S. alone, some 600,000 hospital-based healthcare workers experience occupational, percutaneous injuries annually (King & Strony, 2023). Infectious organisms present in the blood that can cause serious or life-threatening diseases in humans include hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV).
An exposure control plan is essential in a healthcare setting, and as a healthcare professional, you must know your facility's policies. The exposure control plan must describe how an employer will use a combination of engineering and work practice controls, ensure the use of personal protective clothing and equipment, and provide training, medical surveillance, hepatitis B vaccinations, and signs/labels. Engineering controls are the primary means of eliminating or minimizing employee exposure, and safer medical devices, such as needleless devices, shielded needle devices, and plastic capillary tubes, are used.
Should a needlestick or exposure to blood occur, Provide immediate care to the exposure site.
- Wash wounds and skin with soap and water.
- Flush mucous membranes with water.
- Irrigate eyes with clean water, saline, or sterile wash.
Please note that no scientific evidence has shown that using antiseptics or squeezing the wound will reduce the risk of transmission of a bloodborne pathogen. Using a caustic agent such as bleach is not recommended.
A comprehensive exposure prevention plan and strategies significantly decrease the risk of infection from bloodborne pathogens. The risks of exposure with appropriate precautions are low, yet they are real. Understanding how exposure occurs and the risk of exposure is imperative for both the occupational health clinician and the healthcare worker. After occupational exposure to a bloodborne pathogen, the risk of infection depends on several factors, including:
- Type of body substance involved.
- Route of exposure.
- Volume of blood or body fluid involved.
- Severity of exposure.
- Pathogen suspected.
- Degree of viremia (e.g., viral count or quantity of virus in the blood).
- Immune status of the healthcare worker at the time of exposure.
- Was appropriate post-exposure prophylaxis (PEP) used?
Pain Management
The right to be heard when suffering from pain, to be assessed seriously, not to have their pain minimized, and to have appropriate treatment options presented is an essential right for all humans. Some healthcare organizations and health providers forget this foundational ideal in the search for convenience and profit. Do not worry; your eagle-eyed regulatory agency soars, ready to swoop should any of us misplace our first loves.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC LD.04.03.13 | Ongoing education and training on the assessment and management of pain. |
(JCR Staff, 2024j)
Pain may be defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. Pain is always subjective. Pain is whatever the person is experiencing; it says it is, and it exists whenever they say it does. Clients may experience acute, chronic, or cancer (e.g., malignant) pain.
Acute pain follows injury to the body and disappears as healing takes place. Typically, this is not greater than six months. There is an identifiable pathology that accounts for the pain. For example, it may arise from operative procedures or tissue trauma associated with an inflammatory process. It is often associated with objective physical signs such as increased heart rate, hypertension, and pallor (autonomic nervous system activity), giving a visual appearance we associate with being in pain.
Chronic nonmalignant pain is pain that lasts for an extended period, usually greater than six months. There may or may not be a known active pathology to account for the suffering that the individual is experiencing. Chronic pain, in contrast to acute pain, is rarely accompanied by signs of autonomic nervous system activity, leading to many of us doubting the existence of legitimate pain.
Cancer pain may be acute, chronic, or intermittent. It usually has a definable cause, which is usually related to tumor recurrence or treatment.
Pain Assessment
Basic pain assessment is simple, must be performed regularly, and action is planned based on client reports. It makes no difference whether the client is in the hospital, a long-term care facility, a behavioral health facility, an outpatient clinic, or being cared for by a home care agency. No matter where the client is, the intensity of pain should be assessed and documented:
During the initial evaluation of the client
After any known pain-producing procedure
With each new report of pain
At regular intervals when vital signs are taken
At suitable intervals after pharmacologic intervention (60 minutes after oral; 30 minutes after parenteral) or nonpharmacologic intervention to evaluate the current pain treatment plan.
The most widely used measure to assess intensity is the Numerical Rating Scale (NRS), where the client is asked to rate their pain from 0 to 10, with 0 equaling no pain and 10 equaling the worst possible pain they can imagine. Since we have no instrument to objectively measure pain intensity like a sphygmomanometer measures blood pressure, the only valid measure of pain is the client’s self-report (a subjective measure). Sometimes, healthcare professionals may believe they are the best judges of a person’s pain; however, many studies demonstrate that healthcare professionals either overestimate or underestimate a client’s pain.
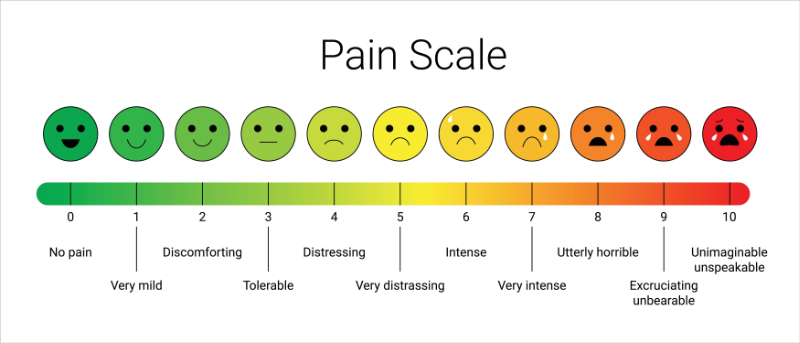
Face Pain Scale
The Faces Pain Scale (FPS) for adults and children can be used for clients who cannot respond verbally and rate their pain numerically. This scale consists of images of faces with various expressions (e.g., smiling, frowning, grimacing). The client selects the face that is consistent with their current pain level.
If a client has cognitive/expressive deficits, observation of nonverbal expression and behavior or report of a family member or significant other needs to be considered when assessing pain intensity.
Each healthcare institution should use a pain intensity rating that will elicit a full assessment. Besides intensity, the complete pain assessment includes the following:
- Location of pain.
- Character or Quality (throbbing, shooting, sharp, cramping, aching, burning, etc.).
- Onset, duration, variations, rhythms (is the pain better or worse at certain times, certain hours?).
- Alleviating factors - what makes the pain better?
- Aggravating factors - what makes the pain worse.
- Effects of pain (impact on daily life, function, sleep, appetite, relationships with others, mood, emotions, concentration, etc.).
Hazardous Flammable Combustible - Liquids, Vapors, and Gases
A major hazard in all hospitals is the widespread use and storage of hazardous, flammable, and combustible liquids and gases. Many liquids have flammable or combustible vapors and can be ignited by a spark from a motor, friction, or static electricity. Handling and storage directions must be followed and are located on the SDS for that material. All flammable liquids should have the following label(s).
 |
 |
|---|---|
 |
 |
Compressed gases are under pressure and flammable, so they must be handled cautiously. An exploding cylinder can have the same destructive effect as a bomb. Storage areas for compressed gas cylinders should be well-ventilated, fireproof, and dry. Cylinders should not be stored near steam pipes, hot water pipes, boilers, highly flammable solvents, combustible wastes, unprotected electrical connections, open flames, or other potential heat sources or ignition. Cylinders should be labeled appropriately. The valve protection cap should not be removed until the cylinder is secured and ready for use.
| Agency Regulation | Ongoing Required Training |
|---|---|
| OSHA 1910.19 | Training at least every three years on safety and health hazards concerning hazardous chemicals. |
| OSHA 1910.101 | Training for staff handling or near where compressed gases are used or stored requires initial training and keeping “current” with safety training. Though training schedules are not specified, annual staff training has been recommended. |
| NFPA 99 11.5.2.1.3 | Continuing education programs shall include periodic reviews of safety guidelines and usage requirements for medical gases and their cylinders. |
(OSHA, 2023a; James. n.d.; NFPA, 2024)
Compressed hospital gases include acetylene, ammonia, anesthetic gases, argon, chlorine, ethylene oxide, helium, hydrogen, methyl chloride, nitrogen, and sulfur dioxide. Acetylene, ethylene oxide, methyl chloride, and hydrogen are flammable, as are the anesthetic agents cyclopropane, diethyl ether, ethyl chloride, and ethylene. Although oxygen and nitrous oxide are labeled as nonflammable, they are oxidizing gases that will aid combustion.
Antineoplastic Drugs, Hazardous Drugs, Toxic Substances
Pharmaceuticals are chemicals. Certain pharmaceuticals have a higher risk of toxicity, both when taken as directed and during incidental exposure. It is important to be aware of high-alert medications such as those identified in the 2016 NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings, which includes such classifications as insulins, opioids, antithrombotic agents, antiarrhythmics, chemotherapeutic agents, chemicals that slow or prevent the formation of clots in the blood (e.g., anticoagulants), and many more.
Exposure to hazardous drugs may occur to clinical and non-clinical workers in the following settings.
- When reconstituting drugs or further dilution.
- When expelling air from syringes filled with hazardous drugs or during the administration of drugs.
- When dust is generated by counting oral doses and tablets from multi-dose bottles or unit-dosing uncoated tablets in a unit-dose machine.
- When crushing tablets to make oral liquid doses.
- When compounding powders into custom dosage capsules.
- When drugs are present on drug vial exteriors, work surfaces, floors, and final drug products (bottles, bags, cassettes, and syringes).
- When handling body fluids, clothing, dressings, linens, and other materials contaminated with body fluids or hazardous drugs.
- When handling contaminated waste at any step of the preparation or administration process.
- When specialized procedures (intraoperative intraperitoneal chemotherapy) are performed.
- When handling unused hazardous drug waste, hazardous drug-contaminated waste, decontaminating, and cleaning drug preparation or clinical areas.
- When transporting infectious, chemical, or hazardous waste containers.
- When removing and disposing of PPE used while handling hazardous drugs or waste.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC NPSG.03.05.01 | Education and training on anticoagulant therapy. |
| OSHA 29 CFR 1910.1200. OSHA 29 CFR 1910.1450(f) |
Training to ensure that employees are apprised of the hazards of chemicals, medications, and vaccines present in their work area. |
(James, n.d.; JCR Staff, 2024h; OSHA, 2023a)
Healthcare workers’ responsibilities concerning antineoplastic and other hazardous drugs include:
- Review guidance documents, safety data sheets (SDS), and other information resources for hazardous drugs handled.
- Be familiar with and recognize sources of exposure to hazardous drugs.
- Prepare these agents in a dedicated area where access is restricted to authorized personnel only.
- Use two pairs of powder-free, disposable chemotherapy gloves with the outer one covering the gown cuff whenever there is a risk of exposure to hazardous drugs.
- Avoid skin contact using a disposable gown made of a low-lint and low-permeability fabric. The gown should have a closed front, long sleeves, and elastic or knit closed cuffs and should not be reused.
- Wear a face shield to avoid splash incidents involving eyes, nose, or mouth when adequate engineering controls are unavailable.
- Wash hands with soap and water immediately before and after removing personal protective clothing, such as disposable gloves and gowns.
- Use syringes and IV sets with Luer-lock fittings to prepare and administer these agents, and place drug-contaminated syringes and needles in chemotherapy sharps containers for disposal.
- When an IV line must be primed with a solution containing hazardous medication, it should be done in a pharmacy.
- When additional protection is necessary, use closed-system, drug-transfer devices, glove bags, and needleless systems within the ventilated cabinet.
- Manage hazardous waste and contaminated materials separately from other trash.
- Decontaminate work areas before and after each activity with hazardous drugs and at the end of each shift.
Clean up spills immediately using appropriate safety precautions and personal protective equipment (PPE) unless the spill is large enough to require an environmental services specialist.
While having current information on all high-risk therapeutics is important, take particular care to be familiar with any specifically called out in regulatory statutes.
Electrical Safety
TJC’s environment of care guidelines, as well as OSHA, mention the electric needs found in today’s health environment. Health workers need to pay special attention to electrical hazards because they work with tools comprised of electrical circuits. Encountering an electrical voltage can cause current to flow through the body, resulting in electrical shock and burns. Severe injury or even death may occur.
| Agency Regulation | Ongoing Required Training |
|---|---|
| NFPA 99 10.5.8 (NFPA National Fire Prevention Agency) |
Healthcare facilities will provide continuing education for installing and maintaining electrical appliances. It does not specify the interval of mandated education; however, yearly is again recommended. |
(UpCodes, 2012)
All equipment brought into a facility must be safety-checked by the engineering department. Violations of standards governing the use of electrical equipment are the most frequently cited causes of electrical fires. Equipment and appliances that are frequently ungrounded or incorrectly grounded include.
- Three-wire plugs attached to two-wire cords.
- Grounding prongs that are bent or cut off.
- Ungrounded appliances resting on metal surfaces.
- Extension cords with improper grounding.
- Cords molded to plugs that are not properly wired.
- Ungrounded, multiple-plug spiders are frequently found in office areas and nurses’ stations.
- Personal electrical appliances brought by the workers from home (radios, coffeepots, fans, electric heaters) that are not grounded, have frayed cords, poor insulation, or are otherwise in poor repair.
Waived Testing
Waived tests are on The Joint Commission hot sheet now, so have your staff prepared. Waived testing is the technical term used for simple-to-use tests with negligible risk of error. What is being “waived” is the on-location clinical laboratory oversight requirements for certain simple tests, not the test itself. Do not worry if the new term used for these point-of-care (POC) tests seems confusing; it is!
| “Under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), simple, low-risk tests can be waived and performed with no routine regulatory oversight in physicians' offices and various other locations”. Tests can be waived under CLIA if they are determined to be "simple tests with an insignificant risk of an erroneous result.” Those testing sites performing without regulatory oversight must hold a certificate of waiver (CW or COW) from CLIA. A valid CLIA certificate is required for Medicare reimbursement. |
(Federal Register, 2022)
| Agency Regulation | Annual Required Training |
|---|---|
| TJC WT.03.01.01.EP.6 | Annual training and competence for Waived Testing |
(JCR Staff, 2024k)
The Clinical Laboratory Improvement Amendment (CLIA) regulates laboratory testing and requires clinical laboratories to be certified; medical laboratories require extensive certificates to do business. Waived testing is also overseen by CLIA and three federal agencies that work together with CLIA to ensure accuracy and exacting standards are met.
- FDA – the Food and Drug Administration
- CMS – Combined Medicare Medicaid Services
- CDC – Centers for Disease Control
Clear documentation of the training each person performing a waived test has completed must be readily available to auditors. This means training for each waived test (e.g., documentation for a blood glucose meter, documentation for fecal blood strips, etc.), not a one-size-fits-all “they had waived test training.” Please don’t shrug this off; over forty tests are currently in the waived category. If you are the “person Friday” in a physician’s clinic, you will need to train, have documentation for each test you use, and show a fresh test completion for every update the manufacturer makes to each specific waived test.
| Agency Regulation | Ongoing Required Training |
|---|---|
| TJC WT.03.03.01 EP.1,3,4 | Education, training, and documented competency for every staff member performing waived testing, every test they do, and every update to that test. |
(JCR Staff, 2024k)
Some waived test helpful suggestions.
- Take advantage of free training offered by manufacturers of tests used.
- Use the manufacturer’s instructions from the most current lot. Instructions change over time, and you are responsible for what is current now, not then.
- Quality control and calibration, as specified by the kit manufacturer, is necessary; do it and document it clearly. Keep those records for two years to meet CLIA requirements.
- When the manufacturer supplies reagents or test kits, do not tamper with them. Health personnel are notorious for doing cost-saving tricks such as cutting a test strip in half lengthwise to get two uses.
- Never use outdated strips or reagents.
- Handle all test kits as the manufacturer recommends. No tucking temperature-controlled reagents in that space alongside the wheezing over-heated refrigerators’ coils, for instance.
- Be sure to follow all regulations that pertain to laboratory testing, such as bloodborne pathogens and hazardous waste handling.
Conclusion
The public sleeps better at night, knowing that healthcare has regulatory guardians assuring quality is being given to them, the client.
While everyone in the health professions works to give the best care possible, we sometimes get distracted. It is good that we have authorities, regulatory agencies, and accreditation organizations looking on from outside the fuss and flurry. They help us stay on the path of evidence-based care and give guidance when we stray.
Annual required training, not from our employer but from organizations with a more global viewpoint, aids us in keeping a solid foundation in our practice of quality client care.
The required annual mandated training changes frequently, so we must stay current with the focus areas of state, federal, and independent organizations to which we owe diligence. This year’s topics may differ slightly or greatly from the previous year. Whichever it may be, we know that proof of training will be required on inspection, accreditation visit, or in our employer’s annual evaluation of our performance and readiness.
Do not fear audit, accreditation, inspection, or survey. Be ready for every surprise visit by giving quality care and having the annual required training completed and safely documented.
References
- Abadie, R. B., Brown, E. M., Campbell, J. R., Alvarez, I. A., Allampalli, V., Ahmadzadeh, S., Varrassi, G., Shekoohi, S., & Kaye, A. D. (2024). Incidence and Risks of HIV Infection, Medication Options, and Adverse Effects in Accidental Needle Stick Injuries: A Narrative Review. Cureus, 16(1), e51521. Visit Source.
- Adler, S. (2023). How often do you need HIPPA training? The HIPPA Journal. Visit Source.
- Atwell, J. (2023). Safe lifting and transfer techniques for caregivers. TheSeniorList. Visit Source.
- Canada, C. & Daitch, L. (2023). Reduce mortality: Prevent surgical site infections. Clinical Advisor. Visit Source.
- CaseText Staff. (2023, November 30). CMS 45 C.F.R. § 164.308(a)(3) & (4). Retrieved from CaseText: Section 164.308 - Administrative safeguards, 45 C.F.R. § 164.308 | Casetext Search + Citator. Visit Source.
- Centers for Disease Control and Prevention (CDC). (n.d.a). Infection Control. CDC’s Core Infection Prevention and Control Practices for Safe Healthcare Delivery in All Settings | Infection Control | CDC. Visit Source.
- Centers for Disease Control and Prevention (CDC). (n.d.b). Transmission-Based Precautions. Transmission-Based Precautions | Basics | Infection Control | CDC. Visit Source.
- Centers for Disease Control and Prevention (CDC). (2024). Global TB Overview. Centers for Disease Control and Prevention. Visit Source.
- Center for Improvement in Healthcare Quality (CIHQ). (2024). CIHQ critical access hospital accreditation standards. Center for Improvement in Healthcare Quality. Visit Source.
- Centers for Medicare & Medicaid Services (CMS). (2023a). State operations manual. Centers for Medicare & Medicaid Services. Visit Source.
- Centers for Medicare & Medicaid Services (CMS). (2023b). Emergency preparedness rule. Centers for Medicare & Medicaid Services. Visit Source.
- Chambers, C. (2023). OSHA’s mandatory annual refresher training requirements. OSHA Training. Visit Source.
- Code of Federal Regulations (CFR). (2024). Title 42. Code of Federal Regulations. Visit Source.
- Correll, R. (2023). 6 Essential vaccines for healthcare providers. Verywell Health. Visit Source.
- Everyday Health Editors. (2023). 9 ways HIV is not spread. Everyday Health. Visit Source.
- Federal Register. (2022). Clinical Laboratory Improvement Amendments of 1988 (CLIA) Proficiency testing regulations related to analytes and acceptable performance. Federal Register. Visit Source.
- GovTrack.us. (2024). H.R. 5067 — 101st Congress: Patient Self Determination Act of 1990. Visit Source.
- Healthwise Staff. (2023). Patient rights and HIPPA. PeaceHealth. Visit Source.
- James, J. (n.d.). OSHA’s required training frequencies. HIS. Visit Source.
- JCR Staff. (2024a, January 14). Information Management. Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024b, January 14). Human Resources. Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024c, January 17). Provision of Care, Treatment, and Services (PC). Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024d, January 14). Transplant Safety. Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024e, January 14). Accreditation Participation Requirements (APR). Visit Source.
- JCR Staff. (2024f, January 14). National Patient Safety Goals (NPSG). Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024g, January 14). Environment of Care (EC). Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024h, January 14). Hospital Crosswalk. Retrieved from Joint Commission Resources E-dition. Visit Source.
- JCR Staff. (2024i, January 14). Infection Prevention and Control (IC). Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024j, January 14). Leadership (LD). Retrieved from The Joint Commission E-dition. Visit Source.
- JCR Staff. (2024k, January 14). Waived Testing (WT). Retrieved from The Joint Commission E-dition. Visit Source.
- King, K. C., & Strony, R. (2023). Needlestick. In StatPearls. StatPearls Publishing. Visit Source.
- Krofcheck, L. D. (2023). Mandatory sexual harassment prevention training. Cipriani & Werner Attorneys at Law. Visit Source.
- McPheat, S. (2023). What’s the difference between Mandatory and Statutory Training? Skillshub. Visit Source.
- Mundey, M. (2023). Complete guide to Statutory and Mandatory Training. Think Learning. Visit Source.
- NFPA. (n.d.). Health Care Facilities Code. Visit Source.
- N.C. Department of Labor. (2022). 29 CFR Part 1910 – General Industry Standards. N.C. Department of Labor. Visit Source.
- Occupational Safety and Health Administration (OSHA). (2023a) Recommended Practices for Safety and Health Programs. U.S. Department of Labor. Visit Source.
- Occupational Safety and Health Administration (OSHA). (2023a). 1910.1450 - Occupational exposure to hazardous chemicals in laboratories. U.S. Department of Labor. Visit Source.
- Occupational Safety and Health Administration (OSHA). (n.d.). Bloodborne Pathogens and Needlestick Prevention. 1910.1030 - Bloodborne pathogens. | Occupational Safety and Health Administration (osha.gov). Visit Source.
- Office of Public Affairs (OPA). (2024). Justice Department Secures Settlement Agreement with State of New York Executive Chamber to Resolve Sexual Harassment and Retaliation Claims Under Title VII. U.S. Department of Justice. Visit Source.
- OSHA Compliance Service. (2022). OSHA training matrix. OSHA Compliance Services. Visit Source.
- SafetyCulture Content Team. (2024). What Everybody Ought To Know About PPE Requirements. Safety Culture. Visit Source.
- Smith, T. (2023). By doctors, for doctors: Ethics guidance now just one click away. AMA. Visit Source.
- The Joint Commission. (2022). Is an enclosure bed, side rails, or hand mitts a restraint? The Joint Commission. Visit Source.
- The Joint Commission (TJC). (2024a). National patient safety goals. The Joint Commission. Visit Source.
- The Joint Commission (TJC). (2024b). Infection Prevention and Control (IC). The Joint Commission. Visit Source.
- The National Institute for Occupational Safety and Health (NIOSH). (2023). Personal protective equipment. Centers for Disease Control and Prevention. Visit Source.
- Ting, D. (2023). The Complete Guide to Protected Health Information (PHI). Tausight. Visit Source.
- UpCodes. (2012). Chapter 10 Electrical Equipment. UpCodes. Visit Source.
- U.S. Dept. of Health & Human Services (HHS). (2023a). HIPPA training materials. U.S. Dept. of Health and Human Services. Visit Source.
- U.S. Dept. of Health & Human Services (HHS). (2023b). HHS Office for Civil Rights issues resources for health care providers and patients to help educate patients about Telehealth and the privacy and security of protected health information. U.S. Dept. of Health & Human Services. Visit Source.
- Warby, R., Leslie, S. W., & Borger, J. (2023). EMTALA and Patient Transfers. In StatPearls. StatPearls Publishing. Visit Source.
- World Health Organization (WHO). (2023). Tuberculosis. World Health Organization. Visit Source.
- Yang, J. (2023). What’s behind an alarming rise in violent incidents in health care facilities. PBS. Visit Source.